This interview is part of a series powered by HLTH and CHIME to highlight key insights and perspectives from key leaders speaking at ViVE
Improving access to specialist care is one of the healthcare pain points that RubiconMD seeks to address. Gil Addo, co-founder and CEO of the company, will speak at the ViVE conference March 6-9 in Miami Beach.
First, it will be part of the discussion, The Next Frontiers in Value-Based Care Technology: How New Population Health, Digital Health, and Next Generation RPM and Diagnostics Technologies Can Accelerate the Value (Presented by Deerfield Management).
He will also participate in a round table, Addressing inequitable access #RuralHealthDilemma. In addition to Addo, other panelists include:
- Nancy Brown, General Partner, Oak HC/FT (moderator)
- Anna Lindow, CEO and Co-Founder, Brave Health
- Dr. Jennifer Schneider, Co-Founder and CEO, Welina Care
- Roshan Navagamuwa, Executive Vice President and CIO, CVS Health
To view the full agenda, Click here.
To register for ViVE, Click here.
To note: This interview has been lightly edited for length and clarity
From the perspective of ViVE, Addo discussed recent behavioral health and rural health initiatives undertaken by RubiconMD as well as its response to Covid-19 and the recent acquisition by Oak Street Health.
How has Rubicon® evolved since 2014? What were some of the milestones you took in the years leading up to the acquisition?
![]()
Gil Addo
The first was to really validate the need we were supporting around value-based care. We have worked hard to develop the payer relationships and partnerships needed to execute this. What we’re doing is more scalable access to specialist expertise, which removes a lot of unnecessary cost from the system… From there, it’s been almost entirely focused on the product and how we innovate in matter of primary care.
We’ve developed a whole bunch of different tools and parts to fit into the primary care workflow more seamlessly. We have developed deep integrations with EHRs to make it easier to submit electronic consultations. We have developed features on mobile [devices]. We have [also] developed a feature to be able to engage other members of a clinic or care team to participate in the process.
We’ve done a whole bunch of stuff from a UI/UX perspective to make it as simple and seamless as possible for primary care.
The other big thing that happened was when we started we had [around] Thirty specialties and sub-specialties. We have determined that one of the most important things to make this as easy as possible for primary care is to have as many specialties as possible on the platform and to be able to really answer all questions. Today, we have 140 specialties and sub-specialties on the platform. It matters because we want primary care [practices] feel like it’s the tool they turn to for all their support and specialist care needs. This includes everything from traditional specialties such as cardiology and dermatology to a wide range of pediatric subspecialties, clinical pharmacy, genetics, and more.
You launched a behavioral health module. Could you give an overview?
We are in the process of commercializing it on a large scale. It’s about being able to provide greater overall support for primary care.
The thing we’ve heard consistently throughout RubiconMD’s history is, “Can you provide better behavioral mental health support?” and our value proposition was that we could reduce costs and strengthen primary care. But if you’re only doing that on the physical health side, but not on the mental health side, you’re not really providing integrated care and support.
We had to invest to really build that. Data suggests it may not be the mental health condition itself [that’s] the high cost factor, but patients with mental disorders cost 6 times more for this system. Primary care is where you can capture, support and manage many of these patients who may never make it to a specialist. We had to create this tool to provide holistic support so that we could build this bridge. It was incredibly well received.
How does this work in practice?
Patients go to their GP, and the doctor can use Rubicon® to get a specialist opinion. We organize a network across the country, and those opinions come back to the primary care clinician within hours. This clinician can then use it to follow up on the patient.
With behavioral health provision, there is a set of patients who are identified as appropriate for collaborative care. They are placed in our program where there is a care manager … who manages this set of patients alongside the primary care clinician. Then we bring a virtual psychiatrist to the care team and they can support the management of these patients longitudinally over time. They can participate in an unlimited number of interactions, we have a collaborative workspace that they can use. They phone each other weekly to discuss cases with the care manager. They can interact directly with the primary care physician when they have questions and, in a limited way, they can also interact with the patient as needed. It means bringing a psychiatrist directly to the care team and [provide] support for this set of patients, the primary care clinician and their team to be able to better manage care.
Additionally, we have created a bespoke registry, to include evidence-based collaborative care tools that care managers can use to manage patients.
So the biggest differences are that it’s both collaborative and longitudinal, compared to online consultations which are pretty much across all specialties, but it’s around specific questions and specific patients.
![]()
Which specialty areas do GPs using your platform use the most for e-consultations?
In the lead, dermatology, cardiology, endocrinology, then hematology-oncology as a joint speciality… OB-GYN, infectiology, orthopedic surgery. Neurology is another big field.
How has your platform adapted to the Covid-19 pandemic?
Virtual was the word of the day when the pandemic hit. We have adapted very well. People didn’t want to be seen unnecessarily in person — we provide a much more efficient way to access the right expertise at the right time.
A lot of people who were on the front line were really struggling… so we had to step in in some areas and just be able to provide the support… It was just crisis mode for a lot of these clinics and organizations.
We have created a specific Covid-19 panel to help people learn how to treat and manage patients with [the condition], how to manage its workforce and personnel. There were a lot of questions [at the start of the pandemic] which now seem to be well accepted behaviors and practices, but no one knew about them at first.
We also do CME so we offer CME across every console. We also have webinars on this – that’s actually another thing that’s changed over the years. We made CME to help train and give clinicians a better understanding of how to meet and manage the needs of their patients with Covid-19.
This also relates to your work on health equity?
The thing we’ve seen during the pandemic…we’ve seen a lot of people looking at health equity and how to support the most vulnerable. I think people really outdid themselves at the time to support vulnerable populations and we are above all a tool to be able to offer more equitable access. We saw a lot of organizations trying to figure out how to address disparities and how to better deal with communities that have fewer resources. We have been able to forge partnerships with many community health centers, many organizations that support underserved communities. We’ve started a rural health initiative, which we’ll talk about at ViVE, so we can support those in rural areas who simply don’t have the same access.
The chronic diseases that drive the cost of health care are the same that disproportionately affect black and brown people. So also solve systemic racism [addresses] health care costs.
Could you tell us a bit about the Rural Health Initiative and what that entails?
We already had large populations that we were supporting in rural areas – we wanted to find ways to better tailor the supply and partner with organizations so we could scale faster in these rural areas. Rather than just developing relationships with every clinic in every geographic area, we wanted to find ways to partner broadly so we could provide support in large geographic areas – areas where there isn’t as much population density, but the same needs for access to specialized care. It was really important for us to find evolving ways to be able to meet this need and fulfill our mission of democratizing medical expertise.
So we launched the Rural Health Initiative to find partners. We have some great partners that we’ll be talking about at ViVE in case studies that have allowed us to do amazing work, in Kansas, in Missouri, work that we’ve done in Texas.
And that brings us back to the acquisition of Rubicon® by Oak Street Health. How did this deal come about?
Oak Street Health is a long-time customer and partner. It started with a discussion of how we’re evolving from what we’re building around behavioral health to being able to provide fully collaborative care and management and really evolved into that vision of virtual specialist care. Can we be every primary care organization’s gateway to specialty care where specialty is virtual first? So to be able to do the things that we’ve done in behavioral health, and to do that in virtually every specialty and create these multidisciplinary care teams that are not just siled in academic medical centers but can be given to every primary care organization across the country. Over time, we believe we can become the specialty care operating system for any organization trying to deliver value-based care. This is really the vision of what we wanted to build. Oak Street Health has clearly been a leader in primary care, so we’ve partnered with them. We are getting very close to primary care centers to be able to innovate to support our customers.
Drawing: Elenabs, Getty Images
]]> 03.11.22 Legislation led by Senators Murkowski, Feinstein, Ernst and Durbin to address domestic violence, dating violence, sexual assault and harassment The Violence Against Women Act (VAWA) Reauthorization Act of 2022, led by U.S. Senator Lisa Murkowski (R-AK), alongside U.S. Senators Dianne Feinstein (D-CA), Joni Ernst (R-IA) and Dick Durbin ( D-IL), goes to the President […]]]>
03.11.22 Legislation led by Senators Murkowski, Feinstein, Ernst and Durbin to address domestic violence, dating violence, sexual assault and harassment The Violence Against Women Act (VAWA) Reauthorization Act of 2022, led by U.S. Senator Lisa Murkowski (R-AK), alongside U.S. Senators Dianne Feinstein (D-CA), Joni Ernst (R-IA) and Dick Durbin ( D-IL), goes to the President […]]]> Credit: Unsplash/CC0 public domain After a year and a half of lockdowns, border closures, mask-wearing and social distancing, and the rollout of the vaccine, Prime Minister Scott Morrison has moved on to what is essentially a “let it rip” pandemic approach. It’s a boost from the government to “open up” and “get back to normal”. […]]]>
Credit: Unsplash/CC0 public domain After a year and a half of lockdowns, border closures, mask-wearing and social distancing, and the rollout of the vaccine, Prime Minister Scott Morrison has moved on to what is essentially a “let it rip” pandemic approach. It’s a boost from the government to “open up” and “get back to normal”. […]]]> This interview is part of a series powered by HLTH and CHIME to highlight key insights and perspectives from key leaders speaking at ViVE Improving access to specialist care is one of the healthcare pain points that RubiconMD seeks to address. Gil Addo, co-founder and CEO of the company, will speak at the ViVE conference […]]]>
This interview is part of a series powered by HLTH and CHIME to highlight key insights and perspectives from key leaders speaking at ViVE Improving access to specialist care is one of the healthcare pain points that RubiconMD seeks to address. Gil Addo, co-founder and CEO of the company, will speak at the ViVE conference […]]]>

 Tallahassee is a long drive from Florida’s Treasure Coast, but it’s a drive I’d happily take to solve one of our state’s most pressing problems. I had the privilege recently of traveling to our state capitol to attend the Florida Senate Appropriations Subcommittee on Health and Human Services for a candid discussion of Florida’s dire […]]]>
Tallahassee is a long drive from Florida’s Treasure Coast, but it’s a drive I’d happily take to solve one of our state’s most pressing problems. I had the privilege recently of traveling to our state capitol to attend the Florida Senate Appropriations Subcommittee on Health and Human Services for a candid discussion of Florida’s dire […]]]>

 COVID-19, in all its dimensions, including incidence, testing, and severity, is known to be associated with social inequalities. 1 Bambara C Riordan R Ford J Matthew F The COVID-19 pandemic and health inequalities. , 2 Wilkins CH Friedman CE Churchwell AL et al. A systemic approach to addressing health inequalities related to Covid-19. , 3 […]]]>
COVID-19, in all its dimensions, including incidence, testing, and severity, is known to be associated with social inequalities. 1 Bambara C Riordan R Ford J Matthew F The COVID-19 pandemic and health inequalities. , 2 Wilkins CH Friedman CE Churchwell AL et al. A systemic approach to addressing health inequalities related to Covid-19. , 3 […]]]> THURSDAY, Feb. 10, 2022 (HealthDay News) — Use of clinical decision support systems (CDSS) is associated with improvements in reversible risk of cardiovascular disease (CVD) in patients with the lowest baseline risk levels. higher, according to a study published online February 4 in Open JAMA Network. Rachel Gold, Ph.D., of Kaiser Permanente Northwest in Portland, […]]]>
THURSDAY, Feb. 10, 2022 (HealthDay News) — Use of clinical decision support systems (CDSS) is associated with improvements in reversible risk of cardiovascular disease (CVD) in patients with the lowest baseline risk levels. higher, according to a study published online February 4 in Open JAMA Network. Rachel Gold, Ph.D., of Kaiser Permanente Northwest in Portland, […]]]> By NICK PERRY and DAVID RISING – Associated Press WELLINGTON, New Zealand (AP) — Entrepreneur Elon Musk is helping to reconnect Tonga to the internet after a volcanic eruption and tsunami cut off the nation from the South Pacific more than three weeks ago, officials say, while repairs to an undersea cable are proving more […]]]>
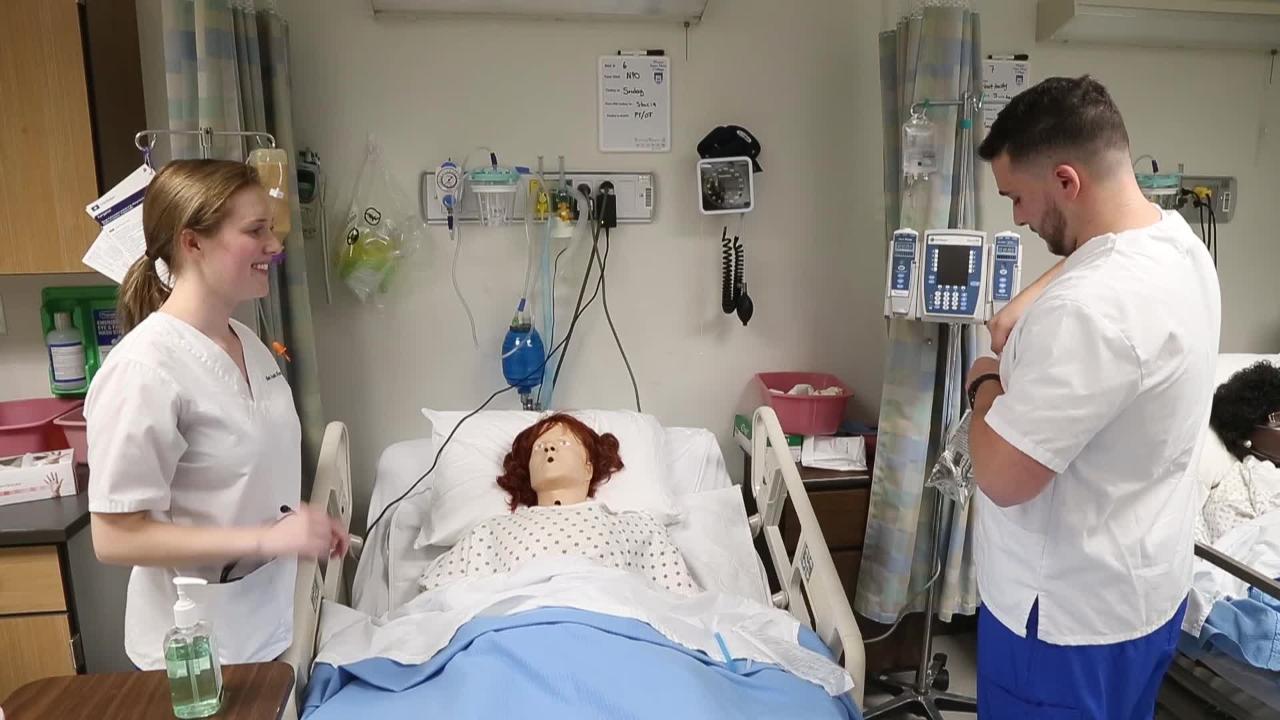
By NICK PERRY and DAVID RISING – Associated Press WELLINGTON, New Zealand (AP) — Entrepreneur Elon Musk is helping to reconnect Tonga to the internet after a volcanic eruption and tsunami cut off the nation from the South Pacific more than three weeks ago, officials say, while repairs to an undersea cable are proving more […]]]> BEND, Ore. (KTVZ) — Central Oregon Community College is hosting virtual information sessions for its nursing and health care programs this month. Sessions include program overviews, structure, duration and cost. The college is hosting virtual information sessions for its Allied Health Programs from 5:15 p.m. to 6:15 p.m. on February 3 and 16. Health programs […]]]>
BEND, Ore. (KTVZ) — Central Oregon Community College is hosting virtual information sessions for its nursing and health care programs this month. Sessions include program overviews, structure, duration and cost. The college is hosting virtual information sessions for its Allied Health Programs from 5:15 p.m. to 6:15 p.m. on February 3 and 16. Health programs […]]]> YORK, Maine — State Representative Patty Hymanson has lived in her family’s home near the York River for about 35 years, but it wasn’t until two years ago that she discovered through testing that the water in his house contained dangerous levels of radon. Hymanson, a neurologist, has since installed mitigation systems that reduce radon […]]]>
YORK, Maine — State Representative Patty Hymanson has lived in her family’s home near the York River for about 35 years, but it wasn’t until two years ago that she discovered through testing that the water in his house contained dangerous levels of radon. Hymanson, a neurologist, has since installed mitigation systems that reduce radon […]]]>



