Washington lawmakers addressed a wide range of health care issues during this year’s legislative session, from staffing shortages to barriers to long-term care, and made progress in addressing equity gaps persistent within hospitals and health systems.
But more work is needed to find solutions to some specific worker and patient safety issues, such as how to better support the state’s chronically understaffed hospitals and overworked employees.
Many mental and behavioral health advocates also came out of the 2022 session wishing more had been done to expand the roles of social workers, therapists and psychologists, although the state’s new supplementary budget, approved Thursday night allocates more than $100 million to help treat behavioral health. labor shortages.
And as the world enters its third year of the COVID-19 pandemic, lawmakers have also earmarked more than $1 billion in unspent federal aid to help stabilize school districts and strengthen education industries. hotels and conventions, the arts sector and small businesses.
Millions will also be invested in cancer research, updating public health data systems, tackling the state’s opioid epidemic, creating more insurance coverage options disease and smoking prevention.
Here’s what Washingtonians should know about this year’s major health care bills and new policies to watch.
COVID Response
Democratic lawmakers this week announced a state budget deal that would use more than $1 billion in remaining federal coronavirus aid, including $345 million to stabilize school districts and $215 million for industries. hotels and conventions, the arts sector and small businesses.
The new supplemental budget also includes $125 million for the state’s current pandemic response, including vaccine distribution, diagnostic testing, disease surveillance and community outreach.
An additional $1.6 billion will be paid into a special disaster response account to help with the ongoing pandemic recovery for families, schools and businesses.
Meanwhile, a bill that would end the COVID state of emergency declared by Gov. Jay Inslee never made it out of committee, nor did a set of bills that would have restored jobs to those who have been fired or resigned due to COVID vaccine mandates.
Hospital/nursing staff
One of the most debated health-related bills this legislative session opened another conversation about state staffing shortages, but ultimately did not pass the Legislative Assembly. House Bill 1868 would have established new staffing standards, including a mandatory nurse-to-patient ratio, better enforcement of meal and rest breaks, and an end to mandatory overtime policies, among other rules.
The state’s three largest health care worker unions fought to keep the bill in hopes of improving retention and workplace safety, but leaders and hospital executives opposed it. the legislation, claiming it would have forced health systems to delay care, eliminate certain services or turn patients around. a way.
“By failing to meet safety staffing standards this session, a handful of lawmakers have allowed hospital leaders to continue to put profits ahead of patient care,” Washington State Nurses leaders wrote. Association, SEIU 1199NW and UFCW 21 in a joint statement this week. “But we are not giving up. We will continue to fight for safe staffing standards, whether in the Legislative Assembly, at the bargaining table or during the vote.
House Bill 2007, which plans to help nurse educators with their student loans, has been passed by the Legislative Assembly and will aim to encourage more people to pursue nursing education, said Representative Eileen Cody, Speaker of the House Health Care & Wellness Committee. in a statement last month.
“Currently, there are 6,000 fewer nurses in the state than we desperately need, but colleges that teach nursing cannot enroll enough new students to fill the gap due to lack of nurse educators available to teach them,” Cody, D-West Seattle, wrote. .
The bill establishes the Nurse Educator Loan Repayment Program as part of the Washington Health Corps, which also operates a separate program that provides loan repayment assistance to health care workers who agree to practice in an “area of shortage” – where medical professionals have been in short supply – for at least three years.
Health Equity
Washingtonians will soon see changes to the state’s charitable care law, which promises free or reduced-cost medical care to low-income patients. The Legislature this week passed House Bill 1616, which requires large hospital systems to provide more financial assistance and increases eligibility for rebates and full waivers of out-of-pocket hospital charges.
Starting July 1, about half of all Washingtonians will be eligible for free or reduced-cost care at hospitals that house about 80 percent of licensed beds.
Under current state charitable care law, individuals whose household income is at or below 200 percent of the federal poverty level are eligible for charitable care. Now, anyone below 300% of the federal poverty level will be eligible for medical financial assistance.
“Under current law, a single parent working two minimum-wage jobs at 50 hours a week was not eligible for financial assistance at hospitals in Washington — that’s not right and it had to change,” he said. State Attorney General Bob Ferguson said in a statement this week.
Lawmakers have also taken steps to address insulin affordability issues by passing Senate Bill 5546, which reduces certain copayments for the hormone from $100 per month to $35 per month. Diabetes advocates said the legislation could do more to address the bigger reasons for high insulin prices – like complicated insurance plans – but many were still in favor of the measure and celebrated its passage.
The law will come into force on January 1.
The state’s birth doulas, which provide physical and emotional support before and after pregnancies, also celebrated a significant victory with the passage of House Bill 1881, which will allow doulas to seek state certification and certification. get Medicaid reimbursement.
The bill will increase access to birth doulas and work to close equity gaps in perinatal care, especially among Black and Indigenous communities, which have been disproportionately affected by perinatal mortality rates. , said supporters of the bill.
Long-term care
Lawmakers this session solidified changes to several state long-term care services and programs, including amending a controversial section of the WA Cares Fund.
Inslee signed House bills 1732 and 1733 in January, a day after Senate lawmakers voted them out of that chamber. The new laws will delay the WA Cares payroll tax for Washington workers and increase the number of people who can claim permanent exemptions to avoid contributing to the program.
The fund was adopted in 2019 as a social insurance program that helps people with difficulty living alone pay for a range of services, such as transport and meal preparation, nursing care and assistance with independent living.
The program is funded by a 0.58% payroll tax on state employees, which was supposed to start earlier this year but is now delayed until July 2023. The delay is seen as a victory for those who fear that some people will pay. in the program, but might never see the benefits.
“By authorizing this extension, access to long-term care becomes more accessible to people closer to retireest,” Cody wrote in a statement last month.
The final supplemental budget also includes funding that tackles barriers to discharge – which have prevented hospitals from offloading patients who no longer need a hospital bed but still need some type long-term care.
The $548.7 million that has been set aside to help patients exit acute care was ‘significantly enhanced’ by Inslee’s hospital staffing initiative, which it announced in January .
“It’s not only better for patients who are otherwise stuck in hospitals, but it frees up hospital resources for patients in need of acute care,” said Zosia Stanley, vice president and associate general counsel at Washington State. Hospital Association, in a press release.
She continued: “With the ongoing response to COVID-19, hospital resources have proven particularly valuable.”
Information from the Seattle Times archives was used in this story.
]]> Nationally, the ACS found that districts with higher uninsured rates also tended to have lower incomes and be in states where government officials chose not to expand health coverage. Medicaid under the Affordable Care Act, the 2010 health care overhaul signed into law by President Barack Obama. The ACA extended Medicaid eligibility to people up […]]]>
Nationally, the ACS found that districts with higher uninsured rates also tended to have lower incomes and be in states where government officials chose not to expand health coverage. Medicaid under the Affordable Care Act, the 2010 health care overhaul signed into law by President Barack Obama. The ACA extended Medicaid eligibility to people up […]]]> BOSTON (AP) — Gov. Charlie Baker on Tuesday unveiled a bill he says would help expand access to primary care and mental health services and help control rising health care and health care costs. prescription drugs. The Republican detailed the legislation during a stop at a health care center in Boston’s Dorchester neighborhood. Baker said […]]]>
BOSTON (AP) — Gov. Charlie Baker on Tuesday unveiled a bill he says would help expand access to primary care and mental health services and help control rising health care and health care costs. prescription drugs. The Republican detailed the legislation during a stop at a health care center in Boston’s Dorchester neighborhood. Baker said […]]]> Washington lawmakers addressed a wide range of health care issues during this year’s legislative session, from staffing shortages to barriers to long-term care, and made progress in addressing equity gaps persistent within hospitals and health systems. But more work is needed to find solutions to some specific worker and patient safety issues, such as how […]]]>
Washington lawmakers addressed a wide range of health care issues during this year’s legislative session, from staffing shortages to barriers to long-term care, and made progress in addressing equity gaps persistent within hospitals and health systems. But more work is needed to find solutions to some specific worker and patient safety issues, such as how […]]]>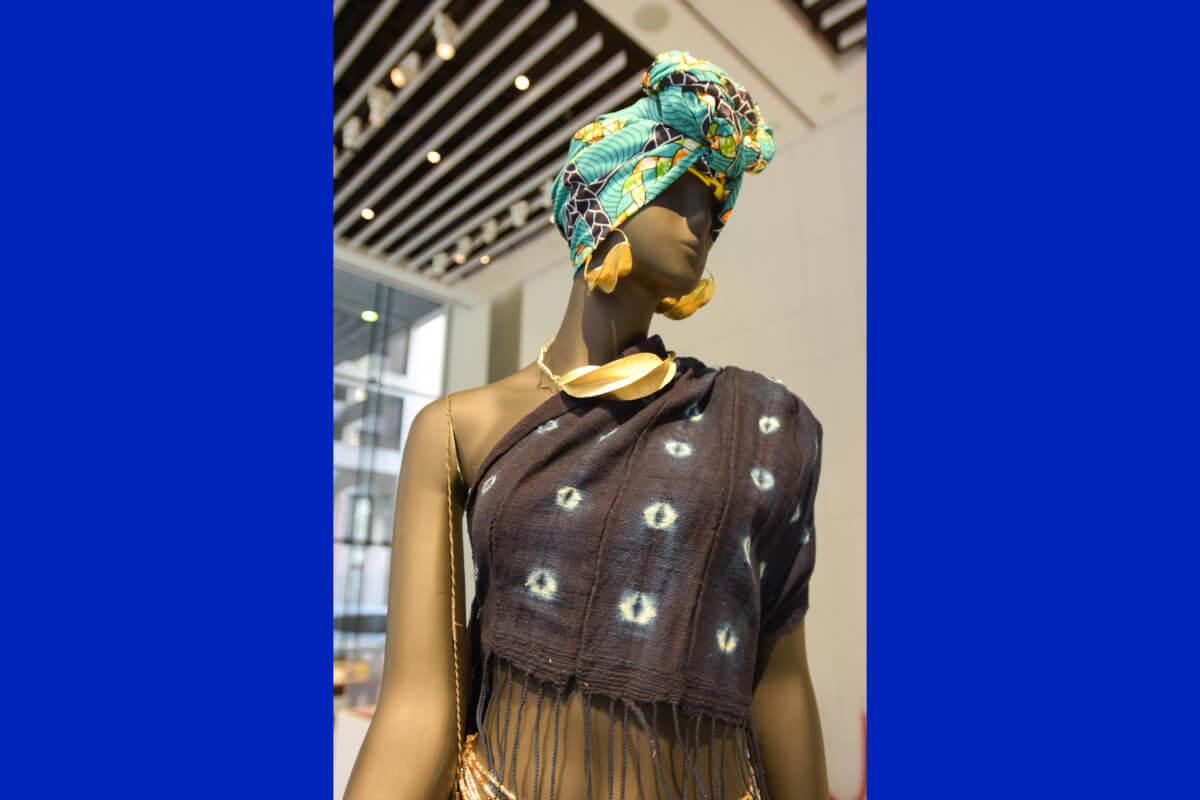 The Fashion Institute of Technology (FIT) Fred P. Pomerantz Center for Art and Design Gallery recently celebrated the opening of Black Health and Wellness, an exhibition of fine jewelry by FIT professor Frank T. Fraley who recognizes the both Western medicine and homeopathic practices across the African Diaspora. With over 30 years of experience in […]]]>
The Fashion Institute of Technology (FIT) Fred P. Pomerantz Center for Art and Design Gallery recently celebrated the opening of Black Health and Wellness, an exhibition of fine jewelry by FIT professor Frank T. Fraley who recognizes the both Western medicine and homeopathic practices across the African Diaspora. With over 30 years of experience in […]]]> 03.11.22 Legislation led by Senators Murkowski, Feinstein, Ernst and Durbin to address domestic violence, dating violence, sexual assault and harassment The Violence Against Women Act (VAWA) Reauthorization Act of 2022, led by U.S. Senator Lisa Murkowski (R-AK), alongside U.S. Senators Dianne Feinstein (D-CA), Joni Ernst (R-IA) and Dick Durbin ( D-IL), goes to the President […]]]>
03.11.22 Legislation led by Senators Murkowski, Feinstein, Ernst and Durbin to address domestic violence, dating violence, sexual assault and harassment The Violence Against Women Act (VAWA) Reauthorization Act of 2022, led by U.S. Senator Lisa Murkowski (R-AK), alongside U.S. Senators Dianne Feinstein (D-CA), Joni Ernst (R-IA) and Dick Durbin ( D-IL), goes to the President […]]]> Credit: Unsplash/CC0 public domain After a year and a half of lockdowns, border closures, mask-wearing and social distancing, and the rollout of the vaccine, Prime Minister Scott Morrison has moved on to what is essentially a “let it rip” pandemic approach. It’s a boost from the government to “open up” and “get back to normal”. […]]]>
Credit: Unsplash/CC0 public domain After a year and a half of lockdowns, border closures, mask-wearing and social distancing, and the rollout of the vaccine, Prime Minister Scott Morrison has moved on to what is essentially a “let it rip” pandemic approach. It’s a boost from the government to “open up” and “get back to normal”. […]]]> By RICARDO ALONSO-ZALDIVAR – Associated Press WASHINGTON (AP) — Legislation to limit insulin costs for people with diabetes is being reactivated in the Senate. Democrats say they want to move quickly, but they’ll need Republican support to get anything through in an evenly divided chamber — and they’re not there yet. Reducing insulin costs has […]]]>
By RICARDO ALONSO-ZALDIVAR – Associated Press WASHINGTON (AP) — Legislation to limit insulin costs for people with diabetes is being reactivated in the Senate. Democrats say they want to move quickly, but they’ll need Republican support to get anything through in an evenly divided chamber — and they’re not there yet. Reducing insulin costs has […]]]>